By Kara Collier, RDN, LDN, CNSC
Maintaining normal blood sugar levels is essential to decreasing your risk for long-term health issues, managing a healthy weight, and feeling good overall. A wide variety of health problems related to glucose level imbalances are a rapidly growing burden for the healthcare system that is reaching epidemic proportions.
CDC’s National Diabetes Statistics Report shows some alarming statistics:
- 34.2 million Americans have either type 1 diabetes or type 2 diabetes. That’s just over 1 in 10 people.
- 88 million American adults have prediabetes. That’s approximately 1 in 3 people, or 34.5% of all US adults. However, only 15.3% of adults with prediabetes reported being told by a health professional that they had this condition!
With such a lack of diabetes management and awareness in the general population, it’s easy for this illness to go untreated. Fortunately, there are more and more options in the market available to the public. Advancements in technology have made tools like continuous glucose monitoring (CGM) devices more readily accessible to the everyday person. This means less reliance on the healthcare system and the ability to take matters into your own hands.
You know your body best. We each have our own unique composition of genetics, diet, and lifestyle, so it goes without saying that our blood glucose levels react differently.
In this article, we’ll take you through what metrics to look out for when measuring and evaluating your blood sugar levels. We’ll also explain how a continuous glucose monitor helps track your data in real-time without fingerstick test strips. You’ll be able to know how to make better diet and lifestyle choices to maintain normal blood glucose levels.
What are normal blood glucose levels?
According to the Mayo Clinic, a normal blood sugar level is less than 140 mg/dL or 7.8 mmol/L. Blood sugar levels less than 100 mg/dL after fasting for at least eight hours are considered normal. If your glucose reading is greater than 200 mg/dL or 11.1 mmol/L two hours after eating a meal, the high blood sugar level could indicate diabetes, which will need to be verified by your doctor. A glucose reading between 140 and 199 mg/dL or 7.8 mmol/L and 11.0 mmol/L could indicate prediabetes.
Which blood glucose values really matter?
There are three general trends that are important to understand when measuring your glucose, whether you are using a CGM or doing fingersticks. By paying attention to these different glucose trends, you’ll be able to get an understanding of how you are doing and where you can improve (everyone always has room for improvement!).
1. Fasting blood sugar levels
This is your glucose value when you are sleeping and without food for at least eight hours. Everyone’s ideal range will be different, but a general guideline is to aim for a value of 70-90 mg/dL.
It will take some time, but focusing on trends will be very helpful here. After a few weeks of collecting data from your continuous glucose monitor, you will start to get a good idea of what your normal is. This will make it easier to identify abnormal days, such as elevated nighttime values after a night of drinking, poor sleep, or high stress.
Note: Sometimes the CGM is calibrated slightly higher or lower than true values (i.e. the values you’d get from a blood test through your doctor). Don’t get too stuck on an exact fasting number. It’s the trend that’s most important.
Why are my fasting glucose values so high?
There are many different reasons why your fasting glucose values could be elevated. One factor to keep in mind is the calibration of the blood glucose monitoring device. The FDA allows CGMs to have up to a 15% variation from what you would receive from a full lab draw at a physician’s office, so your true fasting glucose value may be lower or higher than the CGM reading. The most important thing to consider is the overall glucose trend rather than an exact number. The change in glucose value using the CGM sensor is very precise and reflects real-time changes. With that being said, these are all major factors that may be causing your fasting glucose levels to rise:
- What and when you ate the night before. The content of your meals, portion sizes, and what time they are consumed can have an impact on fasting glucose values. Meals that are high in processed or refined carbohydrates can cause your glucose values to soar during sleep. Additionally, the body tends to not process food as well later in the evening. This means that regardless of what you eat, any food consumption can cause glucose fasting levels to rise if you eat late at night.
- Overall stress levels. Stress causes elevated cortisol levels, which leads to an increase glucose production by the liver. Under normal stressed conditions, cortisol provides the body with glucose by extracting protein stored in the liver via gluconeogenesis. However, over the long term, elevated cortisol levels force the liver to continuously overproduce glucose, leading to increased blood sugar levels, and potentially a diabetic state.
- Low physical activity levels. The effect exercise has on your blood sugar levels will vary depending on how long you are active and what type of exercise you are doing. In general, physical activity makes your body more sensitive to insulin, so it can help lower your blood sugar up to 24 hours or more after working out. When you exercise, your muscles and liver release glucose to be consumed as fuel. When you do moderate exercise for a longer time, like a hike, your body is able to use up a larger amount of glucose. This helps lower your blood sugar levels.
- Poor sleep quality and/or quantity. When you don’t get enough sleep, not enough insulin is released in the body after you eat. At the same time, your body secretes more stress hormones (such as cortisol) to help you stay awake. Cortisol makes it harder for insulin to work properly, so your insulin resistance increases. As a result, too much glucose stays in the bloodstream and your fasting glucose levels become elevated.
- Low-carb diet. It’s fairly common to experience higher fasting and nighttime glucose values if you follow a strict, very low-carb/keto diet for a prolonged period of time. It appears to be a natural adaptation that the body makes to assure there is glucose present for organs that require it, such as the brain.
2. Peak glucose values
Peak glucose values are how high you “spike”, which usually occurs right after a meal. Aim to not spike above 140 mg/dL, and to return to pre-meal glucose values within 2-3 hours after your meal. It’s important to consider how high your glucose goes and how quickly it comes back to normal. You want to avoid dramatic spikes and prolonged increases. A spike every once in a while is not a big deal, but the goal is to minimize the overall occurrence and magnitude so that you don’t enter into hypoglycemia or hyperglycemia.
3. Glycemic variability
Glycemic variability refers to the “swings” in your glucose level. This trend has the greatest implications for health and is especially important to monitor. It’s normal for glucose levels to vary throughout the day, but you want to aim for these glucose “swings” to be gradual with moderate peaks, as opposed to dramatic highs and lows. It may be possible that, after a meal, you only went to 130mg/dL (which is good!), but your pre-meal value was 70, so that would be quite a big swing. Look for a low standard deviation value when looking at your glucose analytics.
If you think a career in holistic medicine is something you would like to pursue, contact us and speak to an admissions representative to get started on your new journey!
How do I naturally lower my blood glucose levels to normal?
If you have elevated blood glucose or big spikes in your glucose levels, we recommend focusing on improving “The Big Four” to get back down to normal levels:
- Nutrition
- Exercise
- Fasting
- Stress
If you’re using a continuous glucose monitor, you will have access to a large amount of real-time and historical data. As you gain a better understanding of what your glucose values and trends mean, the next step is to improve those values and get them to a healthier level.
The most effective ways to manage glucose levels, longevity, and health span can be grouped into what we call “The Big Four“.
1. Nutrition
Your food choices are going to be the primary influence on your health. This is the main pillar that simply cannot be neglected. There is no one-size-fits-all diet, and many plans can fit into a healthy lifestyle. However, everyone can benefit from reducing their intake of refined carbohydrates, added sugars, and processed foods while focusing on consuming high-quality foods.
I used to fear consuming too many carbs and avoided high-sugar foods like bananas. If I was craving carbs, I ate sweet potatoes because they are said to have a lower glycemic index.
However, when I started using NutriSense’s continuous glucose monitor, I learned that my glucose response was the opposite of my initial thinking. Carbohydrate foods I thought were better for me, such as sweet potatoes, have a worse impact on me than bananas.
In my glucose graphs below, bananas lead to a minimal increase in glucose values. I also had low blood sugar levels with beans, legumes, and berries very well. To my great surprise, starchy vegetables (including sweet potatoes) rapidly elevate my glucose values.
Bananas:
Sweet potatoes:
Why do my glucose levels vary so much?
There could be several factors at play here, but in general, there is a lot of variability in glucose responses between person to person. We’re all unique compilations of genetics, epigenetics, environment, and microbiomes that can result in different reactions to the same food. Research has shown that when you give a standardized meal to people, almost everyone has a widely different glucose response with a standard deviation of 31. (Source)
Everyone’s carbohydrate tolerance is different, so that’s why it’s so useful to wear a CGM: you can find out where you lie on the spectrum of general diet advice.
2. Physical Activity
After nutrition, physical activity is the next pillar to master. Include a variety of activities in your routine including stability and mobility, weight and strength training, aerobic exercise, and anaerobic high intensity exercise. Adequate activity doesn’t stop at a hard workout though. Don’t underestimate the importance of daily movement, walking, and limiting sedentary time.
3. Fasting & Meal Timing
Fasting can take on many forms, but experimenting with your eating schedule is a great way to improve your glucose values.
Here are some research-backed experiments to try:
Shorten the hours that you eat to less than 10 hours of the day. Shift your meals towards the beginning of the day, randomly switch up the times that you are eating, and avoid snacking.
Insulin functions according to a circadian rhythm. In general, most people experience the highest insulin sensitivity in the middle of the day, and the least insulin sensitivity in the middle of the night. In fact, insulin sensitivity peaks for most people at noon, and is 54% higher than insulin sensitivity at midnight. (Source)
I find that when I consume fewer carbs at dinner and more during the daytime hours, I improve my glucose responses to those foods. Glucose spikes are minimized and fasting glucose values are lower during the night. If I decide to eat any food, especially carbs, late at night, then I will see the effect on my fasting glucose values all night long.
The glucose graph below shows my glucose levels right before bed. At 11:45pm, I had a bowl of popcorn. As you can see, I experienced an initial glucose spike, and my glucose levels stayed high throughout the night during sleep. Generally, if I consume popcorn during daytime hours, it will give me a small glucose spike, but then come back to normal glucose levels within two hours of eating. When I ate it right before going to bed, my nighttime glucose values stayed elevated until I woke up the next morning. Usually, my nighttime glucose values are between 70–80 mg/dL while I sleep. Imagine if this was happening every night and had no idea! With the CGM providing me with a continuous stream of data, it’s easier to know how to lower my blood glucose back to normal levels.
4. Stress
Stress can be anything that puts the body in a physiological stressful state, which subsequently increases glucose levels. This includes mental stress, physical stress, poor sleep, and illnesses. It’s important to focus on these basics so your body can perform at its best. Elevated cortisol (the stress hormone) can drive up fasting glucose values higher than any other factor. (Source)
When your cortisol levels are consistently high, the brain and liver make extra glucose and decrease your insulin sensitivity so that the excess glucose is available to treat the stress. If this behavior is consistent over time, it dramatically increases our risk of developing chronic conditions such as type 2 diabetes (Source)
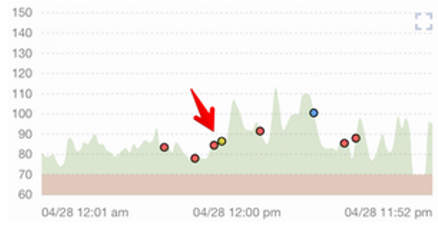
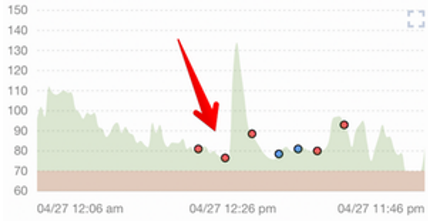
In my glucose graph below, you can see a typical day for me. There is some glucose variability throughout the day, but most of the time, I am staying between 70–100 mg/dL.
This one, however, is a day with similar food and exercise, but when my stress levels were very high. The stress caused my average glucose, fasting glucose, and postprandial glucose levels to all increase. With a CGM system, I’m able to visually see and quantify the effect that stress has on my body, and take action to decrease my glucose levels with a treatment plan.
Note that it’s always best to check with your healthcare professional before experimenting with your CGM.
Featured Posts: