This article is an excerpt from the soon-to-be-published textbook Sports Medicine Acupuncture: An Integrated Approach to Combining Sports Medicine and Traditional Chinese Medicine.
The Chinese term ashi, translated as “that’s the point” or sometimes as another expletive, indicates pain upon palpation of the tissue. Ashi points were first mentioned in the Tang Dynasty text Thousand Ducat Prescriptions and they are still used today to treat musculoskeletal pain. Early Chinese physicians observed that points of tenderness in the muscle were legitimate sites for acupuncture and moxibustion and thus included them in point prescriptions to relieve pain. Many of these points of tenderness responded very well to acupuncture treatment and were subsequently recorded and added to the traditional list of 365 acupuncture channel points. Some of these points were also categorized as
“Extraordinary Points” or simply “Extra Points”. Ashi points may be located anywhere on the body and they become tender when qi and blood are unable to move adequately through the channels and collaterals.
“Tender points can be used as acupuncture points.”
— Ling Shu, Chapter 13
Understanding Ashi Points in CM Practice
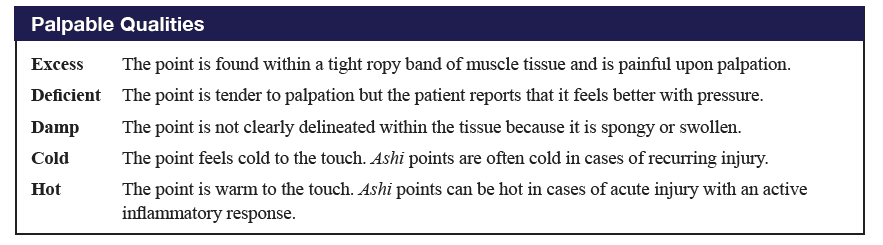
In the presence of any combination of organ disharmony, spondylosis, facilitated segments, painful obstruction syndrome, muscle imbalance, and acute or recurring injury, the channels and collaterals respond in a predictable manner by manifesting ashi tenderness. For example, front-mu and back-shu points become tender from organ pathology, while a cleft-xi point becomes tender from an acute injury. Tenderness of diagnostic ashi points indicates that they should be included in the treatment protocol. In addition to locating ashi points, the practitioner will determine the palpable quality of the point, such as: excess, deficiency, cold, damp, or heat. Figure 1 summarizes the palpable qualities of diagnostic ashi points. We must remember, however, that the palpable quality of the diagnostic ashi point as excess or deficient does not necessarily mirror the excess and deficient diagnosis of the patient’s organ pathology or musculoskeletal injury. In treatment, the quality of the ashi point will guide the practitioner in choosing the appropriate needle technique, angle of needling and depth of insertion for that specific point.
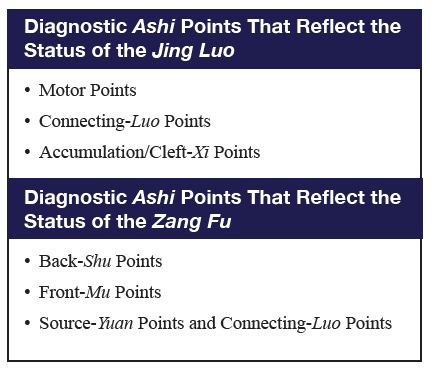
There are many different diagnostic ashi points and for the purposes of this book, the author has divided these points into two larger categories, “Ashi Points That Reflect the Status of the Jing Luo” and “Ashi Points That Reflect the Status of the Zang Fu.” Figure 2 summarizes the types of points within each of these categories.
For the purposes of this article, we will now focus on a common diagnostic ashi point: the muscle motor point. The following information on muscle motor points is a cumulation of the author’s 20+ years of experience in combining Western research, extensive cadaver dissection, and TCM theory.
The Clinical Importance of Muscle Motor Points
The quest to find the optimal location on which to use electricity in the muscle tissue for diagnosis and treatment has been underway for well over a century. Between 1850 and 1930, Duchenne de Boulogne, Jean-Martin Charcot, and Joseph Babinski were some of the first pioneers in neurological medicine to apply electricity to muscles to better understand and treat motor coordination and neuromuscular disease processes.1 Just as technology has advanced over the years, Western biomedical research on muscle motor points has also evolved since the 1930s and has accelerated in the past 30 years. The specialties of neurology and physical therapy have put considerable effort and research into finding the most accurate locations for these points. Transcutaneous nerve stimulation, a common physical therapy modality, requires accurate motor point locations for precise electrode pad placement.2 Motor point locations are also important for neurological interventions such as botulism injection for spasticity due to cerebral palsy and for the location of efficient nerve block injection sites.3-4
Challenges in Identifying Muscle Motor Points
The electrophysiological definition of a muscle motor point is still not universally agreed upon and finding precise motor point locations has proven challenging.5 In fact, the number of motor points per muscle can vary from subject to subject: some individuals have predictable muscle motor point locations and other subjects do not have the same motor point location at all.6-8
This confusion is due in part to the various definitions of a motor point. The motor point has been described as the zone of innervation, which in turn can be defined both as where the motor nerve first pierces the muscle belly (also known as the motor nerve entry point or MEP) and as the location of the terminal end of the motor nerve at the motor-end plate (also known as the intramuscular motor point).9-11 The motor point has also been defined as the cutaneous point, located on the skin above the MEP. Researchers agree that this cutaneous point has the lowest resistance to electrical conductivity in the entire muscle.12-13 The cutaneous point is popularly used for detecting motor point locations with a surface electrode device, although there is a notable lack of consistency from person to person when using this location technique. The thickness and hydration of the subcutaneous layer significantly impacts the effectiveness of the electrical stimulation and detectability of the cutaneous locations of muscle motor points.14
There is a high likelihood that the MEP can be found in the central aspect of the muscle, which is the location that provides the best advantage for neuro-mechanical efficiency to affect the entire muscle.15 When examining muscle motor points in cadaver dissection, there is usually one primary MEP in each muscle. If there are two or more, a frequent occurrence in the infraspinatus muscle, one MEP is usually more reactive to surface electrode stimulation than the other due to the higher quantity of motor and sensory nerve fibers. Once the motor nerve has entered the muscle, in most cases it will bifurcate with one branch travelling in a proximal direction and the other in a distal direction. These proximal and distal branches of the motor nerve traverse the intramuscular spaces until the nerve eventually meets its terminal end at the motor end-plates, which is the location that some refer to as the intramuscular motor point.16-17 The MEP and the intramuscular motor points are both considered to innervate the muscle tissue.
The motor nerve at the MEP is usually larger in diameter and carries a greater quantity of motor and sensory fibers than after the nerve bifurcates in the intramuscular tissue. Although proximal and distal intramuscular motor points can be nearby or a fair distance away from the MEP, research indicates that the MEP, located between the intramuscular motor points, is where the motor nerve endings are most densely populated. This explains why the MEP has the most electrical conductivity.18 The farther the motor nerve travels through the intramuscular tissue, the thinner it becomes. In some muscles, it is so small and indistinguishable that identifying the intramuscular motor points is very difficult, even with the use of microscopic dissection.19-20
Based on the author’s examinations of nerve topography and motor point locations from over 20 years of cadaver dissections, it is safe to say that there are similar and predictable trajectories for the large nerves that traverse the extremities (sciatic, ulnar, etc.), but the point at which the motor nerve branches off the primary nerve to eventually enter the muscle at the MEP varies markedly from specimen to specimen. For example, the author has seen variability in the location where the motor nerve branches off the ulnar nerve to innervate the flexor carpi ulnaris, which has a motor point location of 3-4 cun distal from SI 8 (xiaohai). In certain specimens, a very short collateral branch splits from the nearby ulnar nerve very close to the motor point location and travels at a 70˚-80˚ angle to enter directly into the muscle motor point. In other specimens, the motor nerve branch can split from the ulnar nerve 1-1.5 inches proximal to the motor point location and travel alongside the ulnar nerve until it enters the MEP. In other words, there may be differences in where the motor nerve branches off the primary nerve but the MEP is generally at the same location from specimen to specimen. In addition, the size of the motor nerve that enters the muscle tissue does not seem to be based on the size or sex of the individual. For example, a collateral branch of the median nerve that enters the pronator teres muscle in a 5-foot tall woman can be twice the size as the same nerve of a 6-foot tall man. These types of disparities may be attributable to anthropometric differences or they may be adaptations to the individual’s health and activity level. Other researchers have observed that the sciatic nerve branches to the hamstring musculature can vary randomly in length and size, which can alter the innervation patterning.21-22
Identifying Motor Point Locations
Motor point location references dating as far back as the 1920s were mostly research articles or electromyographic user manuals that provided little more than line drawings of a figure with black dots of approximate motor point locations. These types of drawings were commonly provided with commercially available electrical stimulators. Even by the late 1990s, there were still only a few publications that were helpful in showing the approximate locations of motor points.23-26 When the author went through and cross-referenced these books, it became apparent that there was a lack of consistency between the locations noted in these reference books. For an acupuncturist to effectively use motor points, more precise locations were needed for accurate needle insertion. Around this time, the most commonly used electronic neuromuscular stimulator was the EMS-2A from Medlabs, which used an interrupted galvanic current to test and locate cutaneous motor points. As discussed previously, superficial muscle motor points corresponded to the locations on the skin above the MEP, where an electrical pulse evoked a muscle twitch with the least amount of current.
Starting in the early 1990s, the author used the EMS-2A to begin the process of finding the precise motor point locations on the skin, so that acupuncturists would be able to accurately stimulate these points. The process of testing the points went much like this:
- Once the area of the skin was identified as the probable location of the motor point, the 8 mm circular head from the electrical stimulator was placed on the skin.
- In order to complete the stimulation current loop (monopolar stimulation), a reference electrode was placed over the antagonist muscle unit before the electrical current was initiated.
- A small electrical current was applied from the electrical stimulator to different locations on the skin where the motor point was suspected to lie until it evoked a muscle twitch.
- The twitch response was determined by visual inspection and manual palpation of the muscle and its proximal or distal tendon. When the twitch response was identified, the stimulation current was decreased to a value that still elicited a small response of the muscle in order to further refine the location of the muscle motor point.
- Once the motor point was found and recorded, the author tested the same point location on at least 5 other people to determine the reliability of the location.
In the vast majority of cases, the motor points had consistent locations but there was a small percentage of subjects for which certain motor point locations varied by as much as 0.5 inches from the identified location.
At the present time the author uses a pen electrode to locate cutaneous motor points because it is easier to use than the galvanic stimulator. It is important to remember that surface electrode testing is not useful or reliable for locating muscle motor points in the deeper muscle layers. Motor point locations for muscles such as the hip external rotators and the tibialis posterior are too deep to be tested on the surface of the skin. For these motor point locations, the author relied on research articles to describe the approximate locations of the motor nerve entry points and then, whenever possible, has confirmed these research findings through cadaver dissection.
Are you interested in becoming a certified acupuncture professional?
Visit the links below to explore our specialized acupuncture programs at a campus near you:
Motor Point Locations and TCM Theory
In many Western-based research articles on motor point locations, the measurements are specified through the use of X and Y coordinates that are based on anatomical landmarks. While this can be an efficient way to locate a point, this type of mapping doesn’t offer any additional insights. TCM practitioners have the advantage of a comprehensive system of inter-connected acupuncture points that are categorized and classified in many different ways, including the traditional names of the acupuncture points themselves. This gives the TCM practitioner not only an easy and practical way to find motor points using cun measurements, but in certain cases, especially when a motor point and acupuncture point share the same location, the acupuncture point names or their classifications can provide additional clinical information that enables a more comprehensive, holistic treatment.
For example, the primary motor point for the external oblique shares the same location as LIV 13 (zhangmen). This motor point has a profound effect on correcting pelvic rotations, but if we look at its TCM categorization, we will remember that this point is not only the front-mu point of the spleen, but also a meeting point of the liver and gallbladder channels. Front-mu points are known as “alarm” points, which display ashi tenderness when the corresponding organ is not functioning properly. Knowledge of the crossing points of particular channels is useful because of the point’s influence on those particular channels and organs. So, if the external oblique motor point is tender, the practitioner can understand that not only does the muscle need to be regulated, but there is also a high probability that the patient has some manner of spleen disharmony that may be related to a liver/gallbladder disharmony. There is even the potential that the muscle dysfunction and pelvic rotation is physically affecting the spleen’s ability to function. This is the type of integrative information that practitioners can gain by remembering some of the basics of TCM theory.
In another example, extra point xinfutu shares the same location as the distal motor point of the vastus lateralis muscle. Xinfutu, translated as “new hidden rabbit”, is an extra point located 1 cun posterior to the traditional acupuncture point ST 32 (futu), meaning “hidden rabbit’. The Chinese characters for this point describe how the rabbit, sitting back on its haunches with its knees flexed, is hiding and ready to leap with speed and power. In this case, the name of the point provides us with useful clinical information. After years of experimenting with needling this point, the author suggests that it is best palpated and needled when the knee is flexed between 45˚-60˚. The vastus lateralis is a large and powerful muscle and has two primary MEPs. Xinfutu in particular enhances the explosive nature of knee extension, such as in jumping sports. This point also has an incredible proprioceptive effect on regulating quadriceps muscle firing sequences when combined with the vastus medialis motor points.
In another example where point nomenclature provides additional information, the peroneus tertius motor point occupies the same location as an extra point called naoqing, meaning “brain’s clearing.”. This point is not only useful for musculoskeletal injuries (ankle sprain or foot-over-pronation, for example) but by paying attention to the point’s name and its traditional functions, the TCM practitioner understands that it also has a remarkable ability as a distal point to help with lassitude, amnesia and vertigo.
Ongoing Research and Application in Acupuncture
In addition to over 20 years of the author’s testing, refining, and clinical use, editorial references are provided for the motor point locations that the author has used from 1998 until the publication of this article. Motor point locations can definitely vary and finding the most consistent locations of large diameter motor nerve entry points—those that have the greatest clinical impact when needled—has been a long process. The passion and desire to continue this research has not waned for the author because matching anatomical findings with TCM acupuncture theory and its applications continues to fascinate him.
References
- Clarac, F., Massion, J., & Smith, A. M. (2009). Duchenne, Charcot and Babinski, three neurologists of La Salpetrière Hospital, and their contribution to concepts of the central organization of motor synergy. Journal of Physiology-Paris, 103(6), 361-376.
- Botter, A., Oprandi, G., Lanfranco, F., Allasia, S., Maffiuletti, N. A., Minetto, M. A. (2011). Atlas of the muscle motor points for the lower limb: implications for electrical stimulation procedures and electrode positioning. European journal of applied physiology, 111(10), 2461.
- Lepage D, Parratte B, Tatu L, Vuiller F, Monnier G (2005) Extra and intramuscular nerve supply of the muscles of the anterior antebrachial compartment: applications for selective neurotomy and for botulinum toxin injection. Surg Radiol Anat 27:420–430
- Karaca P, Hadzic´ A, Vloka JD (2000) Specific nerve blocks: an update. Curr Opin Anaesthesiol 13:549–555
- An, X. C., Lee, J. H., Im, S., Lee, M. S., Hwang, K., Kim, H. W., Han, S. H. (2010). Anatomic localization of motor entry points and intramuscular nerve endings in the hamstring muscles.Surgical and radiologic anatomy, 32(6), 529-537.
- Behringer, M., Franz, A., McCourt, M., Mester, J. (2014). Motor point map of upper body muscles. European journal of applied physiology, 114(8), 1605-1617.
- Moon, J. Y., Hwang, T. S., Sim, S. J., Chun, S. I., & Kim, M. (2012). Surface mapping of motor points in biceps brachii muscle. Annals of rehabilitation medicine, 36(2), 187.
- Wang, Z. J., Xing, Y. L., Gao, X., Hu, X. Y., Zhang, L., Li, J., Robinson, N. (2015). Motor entry point acupuncture compared with the standard acupuncture for treatment of shoulder abduction dysfunction after stroke: A randomized clinical trial.European Journal of Integrative Medicine, (7), 26.
- Lee, J. H., Kim, H. W., Im, S., An, X., Lee, M. S., Lee, U. Y., & Han, S. H. (2010). Localization of motor entry points and terminal intramuscular nerve endings of the musculocutaneous nerve to biceps and brachialis muscles.Surgical and radiologic anatomy, 32(3), 213-220.
- An, X. C., (2010) Surg Radiol Anat 32:529–537
- Hwang, K., Jin, S., Hwang, S. H., Lee, K. M., & Han, S. H. (2007). Location of nerve entry points of flexor digitorum profundus.Surgical and Radiologic Anatomy, 29(8), 617-621.
- Chusid, J.G. Correlative Neuroanatomy and Functional Neurology. 15th ed. Los Altos: Lange Medical Publications, 1973.
- Coers C., A.L. Woolf. The Innervation of Muscle. Oxford: Blackwell Scientific Publications, 1959. 3-5.
- Nordander C, Willner J, Hansson GA, Larsson B, Unge J, GranquistL, Skerfving S (2003) Influence of the subcutaneous fat layer, as measured by ultrasound, skinfold calipers and BMI, on the EMGamplitude. Eur J Appl Physiol 89:514–519.
- Seidel, P.M.P., Seidel, G.K., and B.M. Gans. “Precise Localization of the Motor Nerve Branches to the Hamstring Muscles: An Aid to the Conduct of Neurolytic Procedures.” Arch Phys Med Rehabil 77 (1996) : 1157-1160.
- Lee, J. H., Kim, H. W., Im, S., An, X., Lee, M. S., Lee, U. Y., & Han, S. H. (2010). Localization of motor entry points and terminal intramuscular nerve endings of the musculocutaneous nerve to biceps and brachialis muscles.Surgical and radiologic anatomy, 32(3), 213-220.
- An, X. C., (2010) Surg Radiol Anat 32:529–537
- Botter, A., Oprandi, G., Lanfranco, F., Allasia, S., Maffiuletti, N. A., Minetto, M. A. (2011). Atlas of the muscle motor points for the lower limb: implications for electrical stimulation procedures and electrode positioning. European journal of applied physiology, 111(10), 2461.
- Lee, J. H. (2010).Surgical and radiologic anatomy, 32(3), 213-220.
- An, X. C., (2010) Surg Radiol Anat 32:529–537
- Grant, J. C. B. (1989).Grant’s method of anatomy: a clinical problem-solving approach. Williams & Wilkins.
- Seidel, P.M.P., (1996) Arch Phys Med Rehabil 77: 1157-1160.
- Kendall, F.P., McCreary E.K., and P.G. Provance. Muscles Testing and Function. 4th ed. Baltimore: Williams and Wilkins, 1993. 391-392.
- Walthard, K.M. and M. Tchicaloff. Motor points, Electrodiagnosis and Electromyography. 3rd ed. Ed. S. Licht. Baltimore: Waverly Press, 1971. 153-170.
- Warfel, J.H. The Extremities, Muscles and Motor Points. 6th ed. Philadelphia: Lea and Febiger, 1993.
- Warfel, J.H. The Head, Neck and Trunk. 6th ed. Philadelphia: Lea and Febiger, 1993.
Featured Posts:

