By Subhuti Dharmananda, PhD, Director of the Institute for Traditional Medicine (ITM), Portland, Oregon
The Formula and Its Name
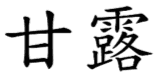
Gan lu yin is a prescription in the Song Dynasty compilation Tai Ping Hui Min He Ji Ju Fang, one of the main sources of formulas used in modern practice of traditional Chinese medicine (TCM). That text includes many formulas with herb-combining characteristics parallel to those found in the Shang Han Lun and Jin Gui Yao Lue, which are also primary sources of ancient TCM prescriptions utilized today.
The name refers to “sweet dew” (gan = sweet; lu = dew). The herbs are to be made in the form of a quickly-prepared cooling drink (yin), rather than taken as a long-boiled hot decoction (tang). Gan lu is a term found in Chinese Buddhist literature, designating those things which are exceedingly wonderful, sometimes referring to food and to healing. For example, Master Zibo Zhenke (1543-1603), a monastic Buddhist knowledgeable about traditional concepts of taste and effect of foods, wrote an essay mentioning gan lu titled “On the Kitchen,” quoted here at some length as this may have value beyond the topic under discussion (1):
The Buddha said, “the place in the temple for preparing offerings and food and drink for the Buddha, the Dharma, and the Sangha [the ‘three jewels’: the Buddha, the teaching of the Buddha, and the community who follow the teaching] is known as the ‘kitchen of accumulated fragrance’”. But if those who prepare food and drink do not understand the three virtues or distinguish among the six flavors, and if their three karmas of body, speech, and mind are impure, then the kitchen ought instead to be called the “kitchen of accumulated filth”. What are the three virtues? They are purity, gentleness, and acting in accordance with the rule [of ethical compassionate behavior]. What are the six flavors? They are plain, salty, spicy, sour, sweet, and bitter. If the food offered to the Buddha and the Sangha is impure and consists of meat and fish [not vegetarian], then the virtue of purity is lost; if it is not fine and pleasing and somewhat astringent [as opposed to oily and rich], then the virtue of gentleness is lost; if it is not made on time, not properly made, not prepared carefully, and not tasted before it is offered to the public, then the virtue of acting according to the rule is lost. If the three virtues are not blended in harmony with the six flavors, the three virtues are lost. The plain flavor is the essence of all flavors. The salty flavor is by nature moist, and it can moisten the muscle and skin. Thus, when blending flavors one should begin with salt. The spicy flavor is by nature hot, and can warm the coolness of the internal organs. Thus the flavor of peppers is called spicy. The sour flavor is by nature cooling, and can release the ill effects of the other flavors. Thus the flavor of vinegar is called sour. The sweet flavor is by nature gentle and it can be gentle on the spleen and stomach. Thus the flavor of sugar is called sweet. The bitter flavor is by nature cold and it is capable of releasing the heat of the internal organs. Thus acridity [a sharp bitterness] is called bitter… When the three virtues are not lacking and the six flavors are not absent, if such food and drink were smelled by the Buddha or entered the mouth of a monastic, it would be like smelling sandalwood and tasting sweet dew. The five internal organs will be balanced and the skin smooth and pleasant, the body comfortable and the mind at peace; [the one who consumes such food and drink will be] externally endowed with physical strength while internally endowed with mental vigor. Endowed with physical strength, the body is healthy. When the mind is endowed with vigor, the spirit will be undisturbed. When the body is healthy, one can advance toward the Way; when the spirit is undisturbed the wisdom of contemplation is easy to achieve. When food does not accord with the rule, then the body sickens and the mind is filled with anxieties. When body and mind are racked with illness and worry, it is impossible to progress toward enlightenment. This being the case, the lives and fates of those practicing the Way are inextricably linked to those in the kitchen…
As can be seen from this explanation, gan lu does not refer to sweetness of taste. Indeed, another similarly named formula, gan lu xiao du dan (antitoxin pills [valued as] sweet dew), is not at all sweet, but rather bitter, sharing in common with gan lu yin two bitter herbs that provide a dramatic effect on damp-heat syndromes: yin chen hao and huang qin. The Buddhist origin of the term gan lu has been associated with the Hindu term amrita, indicating the “drink of the gods,” which is an immortality elixir; in Buddhism it refers to a special drink consumed before certain rituals. Thus, the name of the formula, gan lu yin, is a reference to its remarkable healing qualities, especially as expressed by its balanced and careful formulation approach along the lines Master Zibo has so eloquently explained for the manner of preparing food.
Seeming Contradiction in Diagnostic/Therapeutic Categories
Gan lu yin has the functions of nourishing yin of the organs and clearing damp-heat of the affected secondary parts. Since dampness is a type of excess yin, there would seem to be a contradiction, but this is simply a case of underlying internal deficiency giving rise to a manifestation of external excess. The primary strategy is to resolve yin deficiency of the stomach; but for its intended action, the herbs also are chosen to replenish the lungs. By nourishing the yin of these upper organs, the formula is directed to alleviating heat that manifests above the stomach and lungs. The patient for which the formula is well suited presents signs of stomach deficiency-fire. That fire has combined with the dampness of mucous membranes (e.g., throat and mouth) to yield a local damp-heat syndrome.
The underlying pathogenic factors of yin deficiency and fire may cause symptoms in the stomach, such as recurrent hunger yet difficulty digesting food, but the dominant presentation is experienced as disorders of the throat and oral cavity. A common modern indication is stomatitis, an inflammatory process affecting the mucous membranes of the mouth and lips; additionally, the tongue, gums, and throat can be affected. In the book Chinese-English Manual of Common Used Prescriptions in Traditional Chinese Medicine (2), the primary indications for the formula are: aphthae (mouth and/or tongue ulcerations), foul breath, gingivitis and bleeding from the gums, dry mouth, and sore throat. As fits yin deficiency and damp heat, the tongue appearance is said to be red tongue body with yellow and dry fur, and the pulse is said to be small and rapid. According to the Taiwan Herbal Pharmacopoeia, second edition (3), gan lu yin treats dampness heat of the stomach meridian with fetid mouth odor and sore throat, mouth and tongue sores, gum atrophy and swollen gums. For any individual patient, the disorder may reveal itself through only one or several of these indicators of stomach yin deficiency with damp-heat.
The Formula
Ten herbs are measured in equal proportions and then ground to powder. Each dose is 6 grams of the powder, quickly boiled to make a tea which is somewhat thick, and drunk when cooled. The dose may be repeated two or three times in a day.
- Gan Lu Yin
- mai men dong + tian men dong
- shu di + sheng di
- shi hu
- yin chen hao
- zhi shi
- huang qin
- pi pa ye
- gan cao
Yin Nourishing Part of Gan Lu Yin
The formula has five herbs for nourishing yin and four herbs for clearing heat. The latter are used especially when heat is associated with dampness; additionally, gan cao is used as a soothing agent that also helps unite the two divergent therapeutic principles.


The five yin nourishing herbs are an expansion of a well-known and widely-used pair referred to as “er dong” (the two “dong” herbs): mai men dong plus tian men dong. These are cooling, yin-nourishing herbs that are complemented in many formulations by a mixture of shu di and sheng di so as to further nourish yin and clear heat. The two “dong” are of the lily family, Ophiopogon japonicus and Asparagus lucidus (or closely related species of each). They have overlapping properties and when properly prepared they also have similar appearance, with a translucent yellowish color (image of mai men dong, left; tian men dong, right). Er dong is mainly used for moistening dryness and clearing heat. Frequently, these herbs are combined with phlegm-resolving and antitussive herbs for conditions such as dry cough, dry throat, and dry mouth secondary to lung yin deficiency. The key herb directing the action of gan lu yin to the stomach is shi hu, which is derived from numerous Dendrobium species. Since Dendrobium is in the orchid family, and since orchids are highly restricted in international trade (due to the endangered status of wild orchids), this herb is difficult to obtain outside of China. One of the species used for shi hu was designated Ephemerantha fimbriata, which has since been reclassified into the Dendrobium genus (e.g., as D. fimbriatum or D. plicatile), but because it has been overlooked among the restricted items, this species is sometimes accessible today. Shu di huang (cooked rehmannia) is one of the herbs considered most broadly useful for nourishing yin and blood.
Damp-heat Resolving Part
The key herb of this part of the formula is yin chen hao, which clears heat and dries damp; it is used to alleviate damp-heat affecting the stomach/spleen and the liver/gallbladder (one of its better-known applications is treating jaundice). Together with zhi shi, yin chen hao clears heat and stagnation of the stomach/spleen. The two herbs direct the flow of qi downward while encouraging clear fluid (rather than turbid fluid) to rise up and nourish the chest, neck, and head; these herbs settle the fiery stomach heat that causes symptoms in the oral cavity. They are combined with two ingredients that are especially valued for clearing heat that is damaging the lungs, huang qin and pi pa ye (eriobotrya, also known as loquat); the latter is often used in syrups for dry cough and dry throat, considered useful for both stomach heat and lung heat. Sheng di huang, dried rehmannia, is used to clear heat, and is especially effective for heat affecting the upper body.
Observations
Gan lu yin may get less attention than it deserves, especially outside of China; currently its broadest use is in Taiwan, from which it has come to the West in the form of dried decoctions (granules). The original Western designation for it was “sweet combination”, whereby it loses the important meaning of sweet dew and the name may even deter people who suffer from the ill effects of eating too much sweet foods and beverages. In Chinese Herbal Medicine Formulas and Strategies (4,5), which is often used as a textbook for TCM formula education in the U.S., the formula was not mentioned at all in the first edition, and is given only a single paragraph of explanation in the revised edition. When searching online documents, gan lu yin is usually mentioned only in passing, such as a formula that might be selected for treatment of diabetes, but monographs depicting its nature and use are lacking.
I propose that one barrier to elevating the status of gan lu yin in modern TCM texts is the unusual therapeutic combination of treating both yin deficiency and damp heat in roughly equal measure, a method that is difficult to classify in the modern approach of presenting formulas within a certain set of established groupings for herbal actions. Further, the therapeutic method is one not frequently described in the modern TCM literature, even for conditions like stomatitis. The English-Chinese Encyclopedia of Practical Traditional Chinese Medicine volume on otorhinolaryngology (6) has a section on stomatitis and related disorders; while there is mention of methods of nourishing yin and purging fire, the yin-nourishing portion of the formulas is always rather small compared to that of gan lu yin.
If you think a career in holistic medicine is something you would like to pursue, contact us and speak to an admissions representative to get started on your new journey!
New Applications of the Formula
Herbal prescribers and researchers in Taiwan have found additional value from this formula, especially for aiding cancer patients and those with certain autoimmune disorders. For example, gan lu yin is employed in treatment of liver cancer and one of its mechanisms is proposed to be anti-angiogenesis, that is, having a potential benefit by preventing new vascularization needed for tumor growth (7,8). It is also used as an adjuvant in treating oral cancer, shown to have an effect on inhibiting TNF-alpha, a pro-inflammatory signaling protein that has some tumor necrosis activity but non-essential while chemotherapy is utilized (9). Gan lu yin is used for post-surgery colon cancer patients, to help with reduced food intake (10). For autoimmunity, the formula is sometimes selected for Sjögren’s syndrome (11) and for lupus (12).
References
1. Tidwell S (editor), Many Autumns: A Collection of Chinese Buddhist Literature, 2011 Buddha’s Light Pub., pp 252-254.
2. Ou Ming, Chinese-English Manual of Common-Used Prescriptions in Traditional Chinese Medicine, 1989 Joint Publishing Co., Hong Kong.
3. Huang Liu-huang (Chairperson Editorial Committee), Taiwan Herbal Pharmacopoeia, 2nd Edition (English), 2016 Ministry of Health and Welfare, Taipei, Taiwan.
4. Bensky D and Barolet R (compilers and translators), Chinese Herbal Medicine Formulas and Strategies, 1990 Eastland Press, Seattle, Washington.
5. Scheid V, Bensky D, Ellis A, Barolet R (compilers and translators), Chinese Herbal Medicine Formulas and Strategies (2nd Edition), 2009 Eastland Press, Seattle, Washington.
6. Xu Xiangcai (chief editor), English-Chinese Encyclopedia of Practical Traditional Chinese Medicine, Otorhinolaryngology (v.18), 1990 Higher Education Press, Beijing, China.
7. Ting CT, et.al., Prescription frequency and patterns of Chinese herbal medicine for liver cancer patients in Taiwan, BMC Complementary and Alternative Medicine, 2017; 17(1): 118.
8. Pan CH, et.al., Effects of a Chinese herbal health formula, “Gan-Lu-Yin,” on angiogenesis, Journal of Agricultural and Food Chemistry 2010; 58(13): 7685-7692.
9. Yang JS, et.al., Suppression of the TNF-alpha level is mediated by Gan-Lu-Yin (traditional Chinese medicine) in human oral cancer cells through the NF-kappa B, AKT, and ERK-dependent pathways, Environmental Toxicology 2016; 31(10): 1196-1205.
10. Chao TH, et.al., Prescription patterns of Chinese herbal products for post-surgery colon cancer patients in Taiwan, Journal of Ethnopharmacology 2014 155(1): 702-708.
11. Chang CM, et.al., The Core Pattern Analysis on Chinese Herbal Medicine for Sjögren’s syndrome: A Nationwide Population-Based Study, Scientific Reports 2015; 5: 9541.
12. May YC, et.al., Traditional Chinese medicine therapy improves the survival of systemic lupus erythematosus patients, Seminars in Arthritis and Rheumatism, 2016; 45(5): 596-603.
Featured Posts:
- Oriental Medicine Brings New Life to Chronic Fatigue Syndrome Sufferers
- Properties of Oriental Medicine Herbs
- WHAT IS SYMPATHY: Reflections on Si Jun Zi Tang
- Pacific College of Oriental Medicine to Change Name to Pacific College of Health and Science
- Seasonal Teas: The Best Beverages For Each Time Of Year