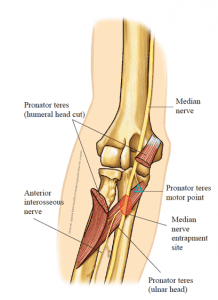
The pronator teres (PT) muscle is located on the ventral aspect of the forearm connecting the radius and ulna. Its length runs obliquely across the forearm and is thicker on the proximal half of the muscle and then becomes a thin, broad tendon in close proximity to its attachment point on the radius. The Latin term teres, which means “round or cylindrical”, describes a large portion of this muscle’s shape, making it easy to locate. The proximal portion of the PT has two heads: the humeral and ulnar. The proximal attachment of the humeral head is on the medial epicondyle and the supracondylar ridge located just above. The humeral head is larger and more superficial than the thinner and deeper ulnar head that attaches to the coronoid head of the ulna. The median nerve travels between these two heads and is susceptible to nerve entrapment, often from an overuse and/or repetitive activity.
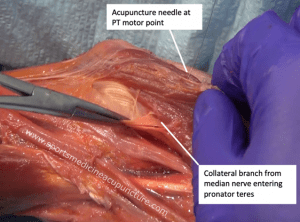
The median nerve innervates the pronator teres. This nerve is a peripheral branch of spinal segments C5-C7, therefore needling the Huatuojiaji points of C4-C6 can help in injury conditions affecting the median nerve. From the brachial plexus, the median nerve travels under the clavicle and pectoralis minor, down the center of the upper arm (P channel) and toward the anterior-medial elbow between the heart and pericardium channels. Between these two channels and approximately 1-1.5 cun distal from the medial elbow crease, just distal to HT 3 (shaohai) and P 3 (quze), the median nerve enters a myofascial space between the two heads of the PT. In close proximity to this location, a large diameter collateral nerve branches off the median nerve and enters into the humeral and ulnar heads of the PT (motor entry point) located at the distal tip of an equilateral triangle drawn from HT 3 and P 3 as shown in this video.
A median nerve entrapment between the two heads of the PT is referred to as pronator teres syndrome (PTS). This soft tissue nerve compression can produce medial elbow pain and paresthesia in the ventral aspect of the forearm. The common mechanism that results in PTS is often from prolonged forearm pronation as seen with musicians and rock climbers, or repetitive pronation and supination movements such as in racket sports. The practitioner will need to palpate the PT motor point (area where the median nerve is primarily trapped) for tenderness, and can further refine the diagnosis using provocative ortho exams (refer to pg. 417 of the Sports Medicine Acupuncture textbook for more information). Some researchers state that pronator teres syndrome is rare (Rasmussen, M. B. 2016), and the author generally agrees that PTS is not an injury frequently seen in the clinic. However, the significance of this anatomical relationship between nerve and soft tissue is that varying levels of median nerve compression can occur and contribute to pain and dysfunction in distal structures, similar to the effect that spondylosis has on the spinal nerve roots, in which mild nerve compression can create signs and symptoms distal to the nerve impingement. Due to repetitive activities, age-related tissue changes, and muscle and postural imbalances, the tissue surrounding the median nerve where it travels through the pronator heads can develop adhesions and fibrotic tissue that compress against the median nerve with varying gradations of pressure.
In injury conditions affecting the median nerve found distal to the elbow, the practitioner should assess for possible nerve compression between the two PT heads that could be a silent contributor to the pain and dysfunction. Although the author could not find any Western biomedical studies to support this hypothesis, Asheghan and his research team did find a correlation between patients with carpal tunnel syndrome (CTS) and those with signs and symptoms of PTS. The author proposes that even mild median nerve compression can contribute to median nerve injuries distal from the nerve entrapment site without having the typical signs and symptoms of PTS, derived from significant clinical evidence from treating the pronator teres motor point for injury conditions distal to the nerve impingement. An example of this is carpal tunnel syndrome: it is common to have a positive Phalen’s test or reverse Phalen’s test become less reactive when repeating these tests after needling the PT motor point. To perform this assessment, the practitioner uses the aforementioned CTS test(s) and examines for a positive result. The practitioner then treats the PT motor point with a perpendicular needle insertion approximately 0.75-1 inch in depth. The practitioner obtains a qi sensation and then withdraws the needle to the subcutaneous tissue ensuring to maintain needle retention. The patient is then asked to repeat the positive ortho exam for CTS with the acupuncture needle in place. The needle should be superficial enough that it does not cause discomfort to the patient while repeating the examination. In many cases, the subjective report of pain and paresthesia from these CTS exams is decreased. The author refers to this process as “acupuncture used as an assessment”.
A Collateral Branch of the Median Nerve
Because the anterior interosseous nerve, a collateral branch of the median nerve that innervates the abductor pollicis longus (APL) and flexor pollicis brevis (FPB) muscles, these tissues should be examined in injury conditions affecting the median nerve. The APL is one of the muscles that is involved in a common wrist injury called de Quervain’s tenosynovitis and the FPL is a major muscle in the stability for the thumb’s metacarpophalangeal joint. Weakness found in the APL muscle during manual muscle testing can be changed after needling the PT motor point (for information on how to perform the APL muscle test refer to pg. 487 of the Sports Medicine Acupuncture textbook). Including the PT motor point when treating de Quervain’s tenosynovitis is recommended. In conditions of the metacarpophalangeal joint, the FPL and PT motor points should be included. In addition, needling the motor points of these muscles, in all of the conditions discussed in this article, can be used in a point protocol to establish communication of the median nerve and myofascial pericardium channel. For more information on the injuries discussed in this article and for motor point locations of the pronator teres, abductor pollicis, longus and flexor pollicis refer to Chapters 8 and 9 in the Sports Medicine Acupuncture textbook.
Are you interested in becoming a certified acupuncture professional?
Visit the links below to explore our specialized acupuncture programs at a campus near you:
More Uses for the PT Motor Point
Inclusion of the PT motor point in the treatment protocol is recommended to help alleviate pain in the same-side rhomboid region and opposite-side neck region (especially affecting the splenii muscles). The postural dysfunction that indicates the use of this point is beyond the scope of this article but the author refers the reader to Brian Lau’s article on the sinew channels for a discussion on this topic.
Because the PT attaches to the medial epicondyle, it should be treated in all cases of medial epicondylitis. The pronator teres motor point should be included in cases of lateral epicondylitis as the pronator teres is an antagonist to the supinator muscle, which can be indicated in this condition. The combination of the PT motor point and supinator motor point is connecting the biao li paired channels of pericardium and san jiao.
The author also uses the PT motor point for opposite-side medial knee pain, especially when aggravated with knee joint rotation. This affect is most likely due to the six division (jueyin) relationship with the liver channel. This point is also effective for pain located in the region of ST 35 (dubi) especially with knee flexion or extension. This affect is most likely due to the midday-midnight relationship with the stomach channel.
References
Rasmussen, M. B., & Deutch, S. R. (2016). Pronator teres syndrome is a rare but important cause of pain in the forearm. Ugeskrift for laeger, 178(46).
Asheghan, M., Hollisaz, M. T., Aghdam, A. S., & Khatibiaghda, A. (2016). The prevalence of pronator teres among patients with carpal tunnel syndrome: Cross-sectional study. International journal of biomedical science: IJBS, 12(3), 89.
Featured Posts:
- Answering Clinical Questions by Investigating the Research Evidence: An Acupuncture/Atrial Fibrillation-Based Example
- Pacific Sports Massage Clinic Scores with Students
- “The Body Remembers”: Alleviating the Long-Term Impact of Injury with Japanese Scar Therapy
- Chinese Medicine & Acupuncture School In San Diego